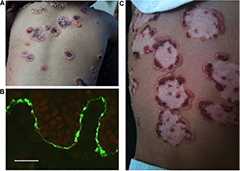
(BMJ)—An 18-mo boy had an erythematous vesiculobullous pruritic rash in the perioral and perineal areas that developed into serosanguineous bullae over ~70% of his body, sparing his mucosa. He was otherwise well and afebrile. Resolving central bullae became circumscribed by small vesicles, giving them a rosette-like appearance. Bx made the dx. What is it?
|
Bullous impetigo
|
|
Chronic bullous disease of childhood
|
|
Bullous pemphigoid
|
|
Dermatitis herpetiformis
|
|
Pompholyx eczema
|
(BMJ)—A 40-yo woman w/ hx of breast CA treated with surgery, chemo, and radiation on tamoxifen for 2 wks presents w/ her skin peeling off, which began when she dried w/ a towel after a bath. ROS: 1 wk malaise/fatigue. Exam: absence of epidermis on ~40% BSA. What is the dx?

|
Paraneoplastic pemphigus
|
|
Pseudoporphyria
|
|
Toxic epidermal necrolysis
|
|
Exfoliative dermatitis
|
|
Staph scalded skin syndrome
|
